Certainly! I will create a complete blog about “Vitamin D Deficiency Symptoms in Hot Countries” in simple English. The main contents of the blog are as follows:
- The Surprising Hot-Country Paradox: Explains why vitamin D deficiency is common despite abundant sunshine, citing global statistics and specific risk factors.
- Why Sun Doesn’t Guarantee Vitamin D in Hot Climates: Uses a table to detail key factors (sun avoidance, skin pigmentation, altitude, heat stress) that inhibit vitamin D synthesis.
- Symptoms That Go Beyond Bones: Describes subtle early symptoms (fatigue, mood changes, muscle issues) and severe deficiency signs (bone deformities, hypocalcemia) across age groups.
- Who is Most at Risk?: Identifies high-risk groups with a table, including veiled/covered individuals, dark-skinned people, office workers, and pregnant women.
- Diagnosis and Treatment: Outlines how to test for deficiency and provides treatment protocols based on severity, including supplementation and dietary advice.
- Practical Prevention Strategies: Offers actionable tips for safe sun exposure, dietary choices, and supplement use tailored to hot climates.
Vitamin D Deficiency in Hot Countries: The Sunshine Paradox and How to Beat It
The Surprising Hot-Country Paradox
When you think of vitamin D deficiency, you probably imagine people living in cold, cloudy regions with limited sunlight. It’s a common misconception that residents of hot, sunny countries automatically get enough of this essential nutrient simply because they live under abundant sunshine. The reality is strikingly different: vitamin D deficiency is a significant public health issue in tropical and subtropical regions worldwide, affecting millions despite the year-round sun.
In fact, a nationwide survey in Colombia—a tropical country—found that nearly a quarter (23.9%) of the population had low vitamin D levels, with certain groups like pregnant women showing even higher deficiency rates. Globally, approximately 1 billion people suffer from vitamin D deficiency, including substantial populations in Middle Eastern, South Asian, and African nations where sunshine is plentiful. This creates a puzzling contradiction: how can people living in some of the sunniest places on Earth become deficient in the “sunshine vitamin”?
The answer lies in a complex interplay of cultural practices, environmental factors, biological adaptations, and modern lifestyles that actually limit sun exposure despite the abundant availability of sunlight. This article will unravel this sunshine paradox, helping you understand why vitamin D deficiency happens in hot countries, how to recognize its subtle symptoms, and most importantly—how to prevent and treat it effectively.
Why Sun Doesn’t Guarantee Vitamin D in Hot Climates

To understand the vitamin D paradox in sunny regions, we need to look at how our bodies produce this crucial nutrient. When ultraviolet B (UVB) rays from sunlight hit our skin, they trigger a chemical process that converts cholesterol into vitamin D3. This seems straightforward in theory—more sun should equal more vitamin D. However, several factors disrupt this equation in hot climates:
Table: Key Factors Limiting Vitamin D Production in Hot Countries
| Factor | How It Reduces Vitamin D | Who Is Affected |
|---|---|---|
| Sun Avoidance | People stay indoors during peak sun hours to avoid heat, missing optimal UVB exposure | Office workers, elderly, children kept indoors |
| Skin-Covering Clothing | Traditional or religious garments block UV rays from reaching skin | Those wearing veils, burqas, long sleeves, or robes |
| Darker Skin Pigmentation | Higher melanin content naturally filters UV radiation, requiring longer exposure | Populations with naturally darker skin tones |
| High Altitude Effects | While higher altitude increases UV intensity, it also leads to behavioral avoidance | Residents of high-altitude cities in tropical regions |
| Heat Stress Response | Physiological stress from heat may increase cortisol, which can break down vitamin D | Everyone in extremely hot environments |
Behavioral sun avoidance is perhaps the most significant factor. In scorching climates, people naturally limit their time outdoors during peak sunlight hours (typically 10 AM to 4 PM), which ironically are the best times for vitamin D synthesis. Many seek shade, stay indoors with air conditioning, or use protective clothing not for cultural reasons but simply for comfort and heat protection. This practical response to extreme heat dramatically reduces effective sun exposure.
Cultural and religious dress practices that involve covering most of the skin further limit vitamin D production. Studies show that individuals who wear traditional covering garments have a five times higher risk of vitamin D deficiency compared to those with similar skin tones who wear less covering clothing. This isn’t limited to any single culture or religion—it affects various communities across hot regions where modest dress is customary.
Darker skin pigmentation, while offering natural protection against UV damage, also reduces the efficiency of vitamin D production. People with darker skin may need 3-6 times longer sun exposure than those with lighter skin to produce the same amount of vitamin D. This biological adaptation, advantageous in sunny ancestral environments, becomes a liability when combined with modern indoor lifestyles.
Interestingly, altitude plays a complex role. Research from Colombia found that for every 100 meters above sea level, the prevalence of low vitamin D increased by 4%. While higher altitude typically means stronger UV radiation, it also often correlates with cooler temperatures that may lead to more skin coverage and less time outdoors.
An emerging theory suggests that heat stress itself might contribute to vitamin D deficiency. When the body is exposed to extreme heat, it activates the hypothalamic-pituitary axis, increasing cortisol production. Elevated cortisol levels may accelerate the breakdown of vitamin D in the body. This means that simply living in a hot environment—even without noticeable sun avoidance—could potentially lower vitamin D levels through physiological stress responses.
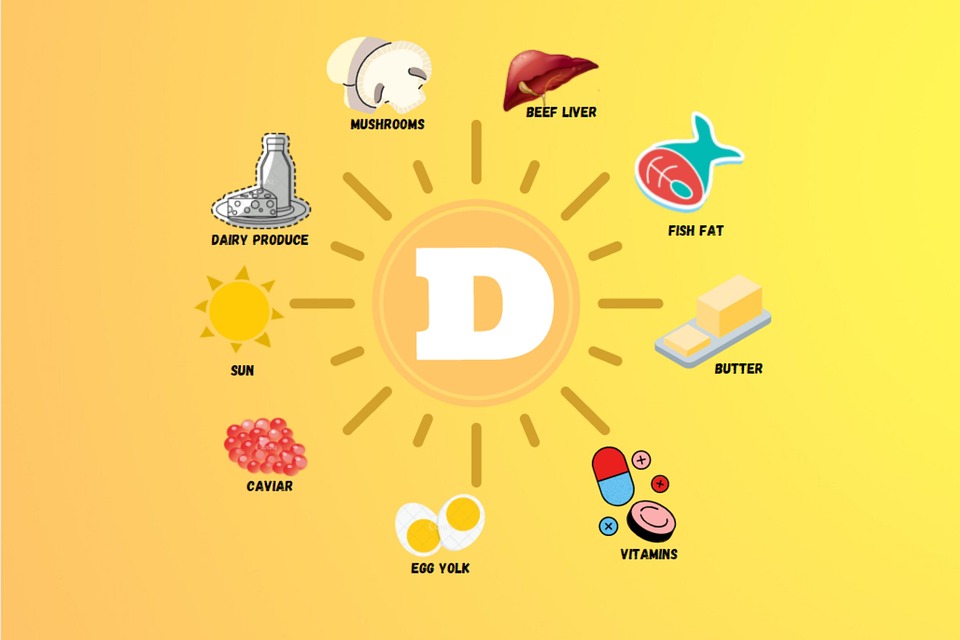
Dietary factors further compound the problem. Traditional diets in many hot countries often lack natural vitamin D sources like fatty fish, egg yolks, and fortified foods. When combined with limited sun exposure, this creates a perfect storm for deficiency.
Symptoms That Go Beyond Bones
Vitamin D deficiency is often called a “silent epidemic” because its symptoms can be subtle, gradual, and easily attributed to other causes. This is particularly true in hot countries, where people might dismiss their symptoms as effects of the heat rather than recognizing a nutritional deficiency. Understanding these signs is crucial for early detection and intervention.
Early and Subtle Symptoms
Many adults with mild to moderate deficiency experience vague, non-specific symptoms that significantly impact quality of life without pointing clearly to vitamin D deficiency:
- Persistent fatigue and low energy that doesn’t improve with rest
- Unexplained muscle weakness, making everyday activities like climbing stairs or getting up from a chair more difficult
- Generalized bone pain or tenderness, often in the back, hips, pelvis, thighs, and ribs
- Mood changes, including depression or low mood, especially during periods of less sun exposure
- Frequent infections as vitamin D plays a crucial role in immune function
- Hair loss in some cases, though this is less common
A compelling real-world example from medical literature illustrates how these symptoms manifest: A 29-year-old woman in a sunny climate presented with increasing pain around her pelvic girdle and upper legs, along with shoulder pain. She found stair climbing “very difficult” and couldn’t rise from a chair without using her hands. Despite living in a region with ample sunshine, her vitamin D levels were undetectably low due to sun avoidance and dietary factors. After treatment, her pain resolved within a week, and her strength returned within weeks.
Signs of Severe Deficiency
When vitamin D deficiency becomes severe or prolonged, more specific and serious symptoms emerge:
In infants and young children:
- Delayed motor development (slow to sit, crawl, or walk)
- Irritability and lethargy
- Muscle cramps or spasms, sometimes progressing to convulsions due to extremely low calcium levels (hypocalcemia)
- Soft skull bones (craniotabes) in infants
In older children and adolescents:
- Bone pain and muscle weakness
- Skeletal deformities including bowed legs, knock knees, or curved spine
- Widened wrists and ankles
- Dental problems such as delayed tooth formation or enamel defects
- Stunted growth or short stature compared to peers
In adults:
- Severe bone pain and tenderness, often in the lower back, pelvis, hips, and ribs
- Proximal muscle weakness affecting the thighs and shoulders, causing a waddling gait
- Fragility fractures from minimal trauma, especially in the ribs, hips, and wrists
- Pseudofractures (Looser zones) visible on X-rays—partial fractures that don’t heal properly
The Calcium Connection

Many symptoms of severe vitamin D deficiency actually stem from secondary hyperparathyroidism—a chain reaction that begins when vitamin D levels drop too low. Vitamin D is essential for calcium absorption from food. When levels are insufficient, the body absorbs less calcium, causing blood calcium to fall. In response, the parathyroid glands work overtime, producing excess parathyroid hormone (PTH). This hormone attempts to normalize blood calcium by leaching it from bones, weakening them over time.
This explains why the most severe consequences of vitamin D deficiency involve bone demineralization: rickets in children (soft, deformed bones) and osteomalacia in adults (bone softening). It also explains muscle symptoms, since calcium is essential for proper muscle function.
Who Is Most at Risk?
While anyone living in hot climates can develop vitamin D deficiency, certain groups face significantly higher risk due to biological factors, lifestyle patterns, or specific life stages. Recognizing if you belong to one of these high-risk categories is the first step toward prevention.
Table: High-Risk Groups for Vitamin D Deficiency in Hot Countries
| Risk Group | Primary Risk Factors | Prevalence Data |
|---|---|---|
| Veiled/Covered Individuals | Complete blockage of UV rays by clothing | 5x higher risk than uncovered peers with similar skin tone |
| People with Darker Skin | Higher melanin reduces UV penetration | May need 3-6x longer sun exposure than lighter skin |
| Office Workers & Indoor Occupations | Minimal midday sun exposure | 35% of adults in sunny regions may be deficient |
| Elderly Population | Reduced skin synthesis efficiency, more time indoors | Up to 90% deficient in some sunny countries |
| Pregnant & Breastfeeding Women | Increased nutritional demands | 6.7% deficient in Colombian study (highest of groups studied) |
| Infants Exclusively Breastfed | Breast milk typically low in vitamin D | Up to 90% deficient in Middle Eastern/South Asian countries |
| People with Obesity | Vitamin D sequestered in fat tissue | 35% higher prevalence regardless of location |
Cultural and religious practices that involve covering the skin create one of the most significant risk factors. Studies across Middle Eastern countries show that women wearing full coverings have particularly high rates of deficiency, often exceeding 80% in some populations. However, it’s important to note that this risk isn’t limited to any single group—anyone who wears sun-protective clothing for legitimate heat protection may face similar challenges.
Office workers and people with indoor occupations represent a growing at-risk population in rapidly developing hot countries. The shift from outdoor agricultural work to air-conditioned office environments means many people now get less incidental sun exposure than their ancestors did, despite living in the same sunny regions. This “modernization paradox” helps explain why vitamin D deficiency remains prevalent even as economies grow.
Pregnant and breastfeeding women have increased nutritional demands, making them particularly vulnerable. Research from Colombia found pregnant women had the highest deficiency rates among all groups studied. This is concerning since maternal vitamin D status directly affects fetal and infant development, with deficiency linked to complications like gestational diabetes, preeclampsia, and low birth weight.
Infants and young children face special risks, especially if exclusively breastfed without supplementation. Breast milk, while nutritionally complete in most respects, is naturally low in vitamin D. In sunny countries, parents may mistakenly believe their children don’t need supplements, not realizing that infants are typically kept out of direct sun for safety reasons.
People with obesity face a unique biological challenge: vitamin D is fat-soluble and can become sequestered in adipose tissue, making it less available in the bloodstream. Those with a BMI over 30 may require higher doses of supplementation to achieve adequate blood levels.
Geographical factors also create unexpected risk patterns. Surprisingly, people living at higher altitudes in tropical countries may be at greater risk. The Colombian study found vitamin D deficiency increased with altitude, possibly because cooler temperatures at elevation lead to more skin coverage. Urban dwellers may also face higher risks than rural residents due to more indoor lifestyles and greater air pollution, which can filter out UVB rays.
Diagnosis and Treatment

If you suspect you might have vitamin D deficiency based on symptoms or risk factors, proper diagnosis and treatment are straightforward but require medical guidance. Self-diagnosis and treatment without proper testing can lead to inadequate correction or, rarely, vitamin D toxicity.
Getting an Accurate Diagnosis
The gold standard for diagnosing vitamin D deficiency is a simple blood test that measures 25-hydroxyvitamin D [25(OH)D], which reflects both dietary intake and sun-produced vitamin D. Different organizations define deficiency slightly differently, but general guidelines are:
- Severe deficiency: <12 ng/mL (<30 nmol/L)
- Deficiency: <20 ng/mL (<50 nmol/L)
- Insufficiency: 20-30 ng/mL (50-75 nmol/L)
- Sufficiency: 30-50 ng/mL (75-125 nmol/L)
For people in hot countries, testing is particularly important because assumptions about sun exposure often lead to underdiagnosis. Many healthcare providers in sunny regions don’t routinely check vitamin D levels, so you may need to specifically request testing if you have symptoms or risk factors.
Along with vitamin D levels, your doctor might check:
- Serum calcium and phosphate (often low in deficiency)
- Alkaline phosphatase (often elevated in deficiency)
- Parathyroid hormone (elevated in response to low vitamin D)
Treatment Protocols
Treatment depends on the severity of deficiency, age, and underlying risk factors. Here are evidence-based approaches:
For severe deficiency (<12 ng/mL or <30 nmol/L):
- Adults: 6,000 IU vitamin D3 daily for 8 weeks, followed by maintenance dose
- Children: 3,000-6,000 IU vitamin D3 daily for 8 weeks, plus calcium supplements
- High-dose weekly options: 50,000 IU weekly for 8 weeks is an alternative approach
For moderate deficiency (12-20 ng/mL or 30-50 nmol/L):
- Adults: 2,000-3,000 IU vitamin D3 daily until levels normalize
- Maintenance after correction: 800-2,000 IU daily depending on ongoing risk factors
Special populations in hot climates often need tailored approaches:
- Veiled/covered individuals: Higher maintenance doses (2,000-4,000 IU daily) may be needed long-term
- People with obesity: May require 2-3 times higher doses to achieve same blood levels
- Elderly: Often need ongoing supplementation of 800-1,000 IU daily due to reduced skin synthesis
Important treatment notes:
- Vitamin D3 (cholecalciferol) is generally more effective than vitamin D2 at raising blood levels.
- Calcium supplementation is usually necessary during treatment since vitamin D enables calcium absorption.
- Follow-up testing is crucial—typically 3 months after starting treatment to check response.
- Improvement in symptoms often begins within weeks, with bone pain improving first, followed by muscle strength.
Practical Prevention Strategies
Preventing vitamin D deficiency in hot countries requires a balanced approach that respects cultural practices, addresses environmental challenges, and fits modern lifestyles. Here are practical, evidence-based strategies:
Smart Sun Exposure
The goal isn’t to bake in the sun for hours—which increases skin cancer risk—but to get sensible, regular exposure:
- Timing matters: 10-30 minutes of midday sun (10 AM to 3 PM), 2-3 times per week. The exact time depends on skin tone—lighter skin needs less time than darker skin.
- Expose adequate skin: Face, arms, and legs without sunscreen during this brief exposure. After this period, use sun protection.
- Cultural adaptations: For those who cover for religious/cultural reasons, exposing forearms and lower legs when in private spaces can help.
- Window exposure doesn’t work: Glass blocks UVB rays, so sitting by a sunny window won’t produce vitamin D.
Dietary Strategies
Since few foods naturally contain significant vitamin D, strategic choices are essential:
- Natural sources: Fatty fish (salmon, mackerel, sardines), egg yolks, liver, and mushrooms exposed to UV light.
- Fortified foods: Look for vitamin D-fortified milk, orange juice, cereals, and yogurt. Availability varies by country.
- Traditional adaptations: Incorporate local fish varieties into regular meals. In landlocked areas, focus on eggs and fortified products.
Supplementation Guidelines
Given the challenges of consistent sun exposure in hot climates, supplements often provide the most reliable solution:
General population prevention doses:
- Infants (0-12 months): 400 IU daily
- Children (1-18 years): 600 IU daily
- Adults (19-70 years): 600 IU daily
- Adults over 70: 800 IU daily
- Pregnant/breastfeeding women: 600 IU daily (some guidelines suggest 1,500-2,000 IU)
Higher-risk individuals in hot countries may need:
- Those with minimal sun exposure: 1,000-2,000 IU daily
- People with darker skin: 1,000-2,000 IU daily
- Elderly: 800-2,000 IU daily
- Those with obesity: 2,000-3,000 IU daily
Community and Policy Approaches
- Healthcare provider education: Ensuring doctors in sunny regions recognize that vitamin D deficiency exists despite abundant sunshine.
- Fortification programs: Implementing or expanding food fortification with vitamin D, as done successfully in many countries.
- Public awareness campaigns: Correcting the myth that “sunny country = no vitamin D problems.”
Conclusion
Vitamin D deficiency in hot, sunny countries represents a significant but often overlooked public health challenge. The sunshine paradox—deficiency despite abundant sun—stems from modern lifestyles, cultural practices, biological factors, and environmental adaptations that limit effective sun exposure.
The consequences extend far beyond bone health, affecting energy levels, muscle function, immune response, and overall wellbeing. Particularly vulnerable groups include those who cover their skin, people with darker pigmentation, office workers, elderly individuals, and pregnant women.
The good news is that both prevention and treatment are straightforward once the problem is recognized. Through sensible sun exposure, dietary strategies, and appropriate supplementation, residents of even the sunniest countries can maintain optimal vitamin D levels.
If you live in a hot climate and experience unexplained fatigue, bone or muscle pain, or belong to a high-risk group, consider discussing vitamin D testing with your healthcare provider. Don’t let the sunshine outside your window fool you—take proactive steps to ensure you’re getting enough of this essential nutrient for long-term health.



